CONDITIONS WE TREAT
Long Jetty and Berkeley Vale Podiatry offers a wide scope of treatment modalities to treat a varying range of foot and lower limb conditions. Our team of podiatrist assess, diagnose and treat;
- heel pain
- plantar fasciitis
- heel fat pad
- achilles tendonitis
- diabetic foot conditions
- arthritic conditions
- occupational injuries
- sporting injuries
- postural conditions
- knee pain
- shin splints
- flat feet
- high arched feet
- severs disease
- sports injuries
- neuromas
- forefoot pain
- bunions
- claw toes
- children foot and leg conditions including; growing pains, sporting injuries, toe walking, juvenile bunions, curly toes, in toe out toe, talipes, sporting injuries, neurological and balance conditions
- ingrowing toenails
- callous and corn debridement
- plantar warts
- fungal nail conditions
DIABETES
Our main concern as podiatrists is how diabetes can affect the delicate blood vessels of the feet. The micro vessels in your feet are responsible for supplying the nerves of your feet, and are vulnerable to high blood glucose levels. When the peripheral nerves have been affected by unregulated glucose levels, your sensitivity to injury can be affected, as well as the ability to effectively heal injuries. This means that you may no longer feel the stone in your shoe if you cut your foot on a shard of glass or if you have a high pressure area under your foot. If these injuries go unnoticed, it can lead to ulceration and possibly infection. A 6 monthly check up with your podiatrist will help to detect any changes in your blood flow and nerve function before they develop into more serious problems.
HEEL PAIN
Heel pain or more specifically plantar heel pain PHP, occurs on the sole of the heel. It is the most common of all foot pain experienced by Australians and can be a very disabling condition. Plantar fasciitis, Heel fat pad syndrome, Tarsal tunnel syndrome, Stress fracture of the calcaneus, Arthritis of the calcaneus, Severs disease, Nerve compression and Bone cysts can all cause PHP.
PLANTAR FASCIITIS
More correctly known as Plantar Fasciopathy. It is the most common cause of PHP (inflammation of the thick fascia that runs along the base of the foot) the pain is most persistent in the morning on rising, it usually lessens and then worsens again through the day or after the day when rising from sitting in the evening. The exact cause of plantar fasciitis is still undecided.
The most successful treatment is multifaceted, reducing the forces exerted along the length of the plantar fascia and at its insertion at the heel bone will assist in reducing symptoms, this can be achieved by taping initially, if pain persist an orthotic is prescribed. Stretching the plantar fascia and the calf muscles is essential to help lengthen these structures, wearing supportive footwear with a low heel will also assist in reducing the pain.
HEEL FAT PAD SYNDROME
Presents as pain more on the outer side of the heel especially when the heel hits the ground when walking or running. The fat pad loses its elasticity as we age and pain may develop following continual heavy loading in unsupportive or non-cushioning footwear or following a high impact landing onto the heel pad, as in a fall or using incorrect technique in high impact sports like netball, long distance running, triple jump or parkour. Confirmation on MRI will display signs of swelling of the fat pad. Treatment is RICE ( rest, ice compression and elevation) strapping and the prescription of silicone gel heel pads.
INGROWING TOENAILS
Ingrowing toenails are a common and very painful condition that can limit your daily activities. You may have inherited your nail shape, some families have nails that are shaped either very flat known as “spoon shaped” nails or they are very curved known as “involuted” nails, both these nail shapes are prone to developing ingrowing toenails. The nail grows into the skin, causing, pain, inflammation, and sometimes infection.
Our podiatrists will discuss with you the most appropriate treatment options.
SPORTING INJURIES
A significant proportion of sporting related foot and limb injuries are directly attributable to impaired foot function and poor or incorrect technique. The bony structures and soft tissues of the feet and legs are vulnerable under extreme forces exerted throughout high repetitive impact activities. Our podiatrists are experienced in the study of biomechanics of the lower limb and will examine, assess and diagnose biomechanical malalignments that place the foot and leg under stress.
Poor foot function and/or technique can result in issues in one or more areas of the feet and legs.
Common injuries of the foot are; stress fractures of the metatarsals, metatarsalgia, plantar heel pain, longitudinal arch pain, turf toe pain.
Common injuries of the leg are; anterior shin pain, stress fracture of the tibia, compartment syndrome, proximal achilles pain, posterior tibial tendonitis.
Common injuries of the knee are; retro patella pain, medial knee pain, patella-tibio tendon pain, ilio-tibial band syndrome, tibio-fibular arthralgia.
CHILDRENS FOOT AND LEG CONDITIONS
Will vary just as adult’s foot ailments vary. Children can develop skin and nail problems to more complex and painful conditions involving developmental or postural variances. Skin and nail conditions will be treated in a gentle and caring manner and we will endeavour to offer pain free treatment options. For more complex issues our podiatrists will assess your child’s feet in relation to the position of their legs, hips, pelvic and spinal positions. A history of your child’s developmental years will be taken from birth through the developing years. Footwear advice for your child’s growing feet can be beneficial to assist with creating the best environment for your child’s foot and leg development.
Our podiatrist can help If you notice:
- rashes or hard skin on your child’s feet
- red or painful toenails
- variations in shoe wear patterns
- toe walking/in toe or out toe walking
- severe flat or high arched feet
- your child complains of recurring pain in the legs or feet
- your child does not look symmetrical
- you notice bumps or lumps on your child’s feet
- your child’s toes are clawing or curling under or over
- if your child frog sits
- your child has trouble balancing, running, hopping, skipping
OCCUPATIONAL INJURIES
Whether you are in retail and your feet ache all day from standing or you are a tradie who is suffering due to heavy repetitive work or a school teacher who walks all day long. Our podiatrists will perform a biomechanical assessment to analyse the cause of your problem and they will provide the appropriate advice and prepare a treatment regime for you. Your footwear may need changing in addition to exercises, stretches and/or orthotics. If you have had a work place injury Long Jetty/Berkeley Vale Podiatry are registered to treat clients through workers compensation claims. Advice on prevention can be offered to your place of work on your request.
KNEE PAIN
There are many and varied reasons why you can develop knee pain. Our podiatrists can assist you when your knee pain is due to postural malalignment of the lower limbs and feet. A biomechanical assessment will determine where the alignment issue is and what is causing it, and a treatment regime will be individualised for you.
Adolescent knees can be vulnerable to stress and become painful due to a combination of high activity, growth and an influx of hormones. Weak muscles and pronated feet can result in painful knees as can degeneration of the knee joints which commonly occurs in later life.
Referral onto your GP or a sports doctor may be necessary if the condition has developed due to an upper body problem or a systemic disease.
SHIN SPLINTS
Also known as Medial Tibial Stress Syndrome (MTSS), describes a pain that presents in the lower two thirds of the shin. The pain is caused by repeated damage to the muscle's connective tissue that surrounds the tibia. Shin splints present in runners and sports people who participate in running and jumping sports such as netball, basketball, tennis, football and athletics.
Biomechanical malalignment may contribute to the development of MTSS, an increase in pronation of the foot whilst running will overload the muscles of the lower leg. When there is an increase in the load exerted onto the muscles of the leg the muscle will fatigue easily and will not absorb shock adequately, in turn this can place undue stress on the bone at the junction where the muscle connects. This stress is associated with the onset of MTSS. Muscle imbalance, including weak core muscles, inflexibility and tightness of the calf muscles, (gastrocnemius, soleus, and flexor digitorum longus) can increase the possibility of shin splints.
ACHILLES TENDONITIS
Achilles tendonitis is inflammation of the Achilles tendon either at its insertion onto the heel bone (insertional achilles tendonitis) or along the length of the tendon (non insertional Achilles tendonitis). The main symptoms are pain and swelling at the back of the heel and the area is often warm and tender to touch. Footwear may irritate the swollen area. Limping whilst walking or whilst participating in sports or at work is common. The cause of Achilles tendonitis is multifactorial, there is often a biomechanical malalignment of the foot and leg and a tightness and or weakness in the calf muscles.
The condition can be triggered by an increase in high acceleration and multidirectional activities, increases in activities too rapidly and repetitively and/or using inappropriate or worn footwear for the activity. Aging increases your risk of developing Achilles tendonitis as the integrity of the tendon is compromised. Our podiatrist will provide combination therapy to treat Achilles tendonitis.
Firstly, activity modification is essential, reduction or cessation of the activity which is irritating your tendon, allowing it to begin to repair and heal.
CORNS AND CALLUSES
Corns and callous ( Helloma durum, known as hard corns, Helloma Millaire known as seed corns, Helloma Mollaire known as soft corns and callous is known as Hyperkeratosis) are a build up of thick skin that grows in areas of high pressure. A callous is a diffuse area of thick skin, whereas a corn is a more concentrated area, usually with a small centre or core. Corn and callous may become painful, and if left untreated may develop an underlying wound.
Corn and callous are formed by increased pressure and friction, and most commonly found over bony prominences, especially in the case of any deformities such as bunions or hammer toes.
Biomechanical malalignment of the joints of the feet will lead to an increased pressure and friction during activity, the skin over the bony prominences and the weight bearing areas of the feet are at high risk particularly with high impact activities such as walking and sport, manual work, or wearing poorly fitting or high heeled footwear. There are some health conditions ( e.g. vascular disease, diabetes, psoriasis, rheumatoid arthritis, dermatitis, smoking and some chemotherapy drugs) that can lead to insufficient blood flow and or fragile skin placing the individual at a higher risk of developing pathologic corns and callous.
Removal of corns and callous by a podiatrist is simple and pain free, offering immediate relief. It involves parring the hard skin away with a scalpel. Soft padding may be applied to the feet in the short term following the treatment.
Our podiatrist will inform you on how to reduce corns and callous in the future, by ensuring you are wearing appropriate and correctly fitting footwear, or by prescribing pressure offloading innersoles, orthoses to realign poor foot structure and function and /or digital devices that can be custom made or premade from our product stand.
Daily care using a moisturiser and a pumice stone or file will go a long way to improved skin quality.
FUNGAL NAIL INFECTIONS
(Onychomycosis) occurs when fungi invade the toenail or fingernail and/or the skin under the nail (nail bed). It can cause nails to crack or thicken, or become discoloured, streaked or spotted. Fungal Nail Infections: (Onychomycosis) occurs when fungi invade the toenail or fingernail and /or the skin under the nail (nail bed). Toe nails are more commonly affected than fingernails, because they grow very slowly, allowing the fungi more time to develop. As a result, toenails require longer treatment time than fingernails do.
Treatment: Onychomycosis is treated with antifungal medication. A nail lacquer is usually the first line of treatment. The lacquer is applied to the nail, the frequency of application will depend on the product advised. Occasionally the nail may need to be removed.
PLANTAR WARTS
Plantar warts are a viral infection of the skin (Verrucae Plantaris) they can occur singularly or in clusters, known as mosaic plantar warts and are caused by the Human Papilloma Virus. They are the most common viral infection of the skin. The HPV thrives in warm moist environments, such as bathrooms, areas around swimming pools and public change rooms. The virus infects the epithelial tissue of the skin and it can spread to adjacent sites on the feet. The warts are demarcated areas of thickened skin, they are often painful to walk on and have tiny black dots in them. Squeezing the sides of the wart will cause pain. Our podiatrist can offer to treat your wart in several different ways. The size and position of the wart or warts and the age and activity levels of the client will help to determine which type of treatment is best for you.
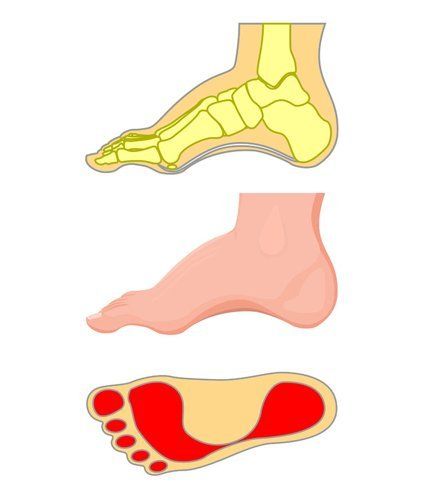
FLAT FEET
Flat feet (pes planus) are identified by the obvious low profile arch or absent arch. Pes Planus are classified as congenital or acquired (to be born with or develop through life) and are not always problematic. A large percentage of people with pes planus are pain free (asymptomatic).
Symptomatic (painful) pes planus are treatable, our podiatrist have a high rate of success in relieving the symptoms. Painful pes planus can develop due to numerous reasons, a typical asymptomatic pes planus may become painful due to an increase in the forces placed on the soft tissues and the joints of the feet resulting in strains. Left untreated inflammation will develop in the numerous small joints and soft tissues that make up the arch of the foot. Increased forces can be due to a sudden increase in high impact activity such as a high volume of running, playing netball, a longer than normal beach walk, heavy lifting or gardening, a change in occupation from sitting to standing, or even painting for long periods of time on a ladder.
An increase in body weight and the use of unsupportive shoes can also be a contributing factor. A tear or dysfunction in the tibialis posterior tendon can lead to the development of a painful one sided flat foot. Several medical conditions can lead to the development of symptomatic pes planus, conditions such as Rheumatoid Arthritis, Diabetes or Stroke.
Our podiatrist will assess and discuss with you what options are best suited to you and your condition. Treatment might involve activity modification, footwear modification, exercises, stretches and/or the prescription of soft or firm orthoses or orthoses with ankle braces for the more severe cases.
HIGH ARCHED FEET
Also known as Pes Cavus are characterised by an increase in arch height and an arch that does not flatten when weight bearing. Pes Cavus tend to be rigid feet and as the arch does not flatten on weight bearing they cannot absorb shock adequately on running and walking. Injury to pes cavus feet typically develop due to increased plantar pressures (sole of the foot) due to poor shock absorption and a reduction in ground contact area. Both the heel and the forefoot fat pads can become irritated by landing hard through running or jumping from a height. Strain on the plantar fascia can develop due to a bowstring type stress that is exerted on the soft tissue of the plantar fascia throughout high impact activities. Shearing stresses placed on the skin of the forefoot pad can result in metatarsal joint pain and inflammation, painful callous and corn may also develop. The Pes Cavus foot type is prone to ankle joint pain and achilles tendonitis due to the poor shock absorption coupled with the position of the ankle joints in relation to the foot. Treatment is varied and will be determined by the severity of the condition.
CLAWED OR HAMMER TOES(DIGITS)
Clawed digits can be a very painful condition and are often associated with the development of corns over the bony prominences as footwear can irritate the deformed joint. Our podiatrists will assess your feet and can determine why you have developed clawed digits and what treatment is best for your individual needs.
Why do claw/hammer toes develop?
There are three common reasons why claw toes develop. The first is due to what we call flexor stabilization, this usually develops in someone with a low arch (flat foot) the small muscles of the feet have become weak and cannot stabilise the foot well through standing and walking. The muscles that control the toes are over working to assist the flat foot lift the arch throughout the walking cycle.
The second is known as extensor substitution
and is the most severe of the clawed digit deformities, the main muscle at the front of the shin which crosses the ankle joint is unable to flex the ankle adequately for walking, the muscles that flex the toes need to over work to lift the foot for ground clearance creating flexion deformities (clawed toes) in the feet. Feet which are at risk are very high arched feet, feet with ankle joints that cannot flex to 90 degrees and feet with spasticity of the ankles.
Thirdly there is flexor substitution, this develops due to weak calf muscles and weak (intrinsic) muscles in the deeper layers of the feet. The muscles of the digits are once again trying to assist the weaker leg and intrinsic foot muscles.
BUNIONS
Are the end stage of a foot deformity known as Hallux Abducto Valgus and our podiatrists can offer a variety of treatment options. The increased risk factors for developing bunions are hereditary, low arched feet, hypermobility of the ligaments of the feet, increased time spent on the forefoot (as in high heels or activities such as performing ballet), rheumatoid arthritis.
Bunions develop due to muscle imbalances in the small muscles of the feet due to poor alignment of the joints coupled with the subsequent increased stress placed on the forefoot. The muscle imbalances cause the 1st metatarsal bone to deviate outwards and the great toe to deviate inwards. The increased stress on the bones result in new bone being laid down around the joint called a bony exostosis, in time this may advance into osteoarthritis. The final stages involve the 2nd toe crossing either over or under the great toe and typically inflammation of the soft tissues over the joint. Inflammation and irritation are often associated with the development of a bursae (sac of fluid) over the joint.
Bunions can create great distress due to the pain and disfigurement that they cause. Footwear fitting can become difficult and many shoes cannot be worn or are painful to wear for even a short period of time.

FOREFOOT PAIN
Can be mild to severe and at times disabling. There are numerous reasons for the development of forefoot pain. Excessive stress on the small joints of the forefoot throughout standing, walking and high impact activities can lead to forefoot pain. Excessive stress in the small joints and surrounding soft tissues of the forefoot can develop due to malalignment of the forefoot, poor or incorrect footwear for the chosen activity, poor sporting technique, continual running on hard surfaces, arthritis, corns and callous, plantar warts, poor blood supply, diabetes and changes in the integrity of the skin and soft tissues due to aging.
FALLS ASSESSMENT
Are a comprehensive assessment to calculate your risk of having a fall.
The assessment involves observations on muscle strength and your balance. A muscle strengthening and balance exercise program will be provided, activity modification may also be advised. Advice on the most appropriate footwear for you and your selected activities will also be provided. Both verbal and written advice on falls prevention will be presented at the time of your assessment. A comprehensive report will be forwarded to your GP.